Learn & Go With Dr. Laurie
How to Prevent a Cranial Cruciate Ligament (CCL) Rupture
This is the first part of preventing Cranial Cruciate Ligament (CCL) rupture, and I’m showing you the first two signs that a dogs CCL is in danger of rupturing. Both in regards to inflammation.
Let’s discuss two key indicators that may suggest risk that a dog's Cranial Cruciate Ligament (CCL) will rupture; joint fluid thinning and increased volume of fluid in the joint. In our video, I will show you how to test for each of these indicators.
Cranial cruciate repair is so common now that 50-85% of all canine orthopedic surgeries performed each year are to repair ruptured CCLs, making it the most common orthopedic surgery done by orthopedic veterinary surgeons.
When I graduated from veterinary school in 1992, CCL tears were typically believed to be caused by trauma. However, today, we see that breakdown of the ligament, secondary to inflammation, is more frequently to blame.
Following that train of thought, if we can minimize or eliminate inflammation in the stifle, we can reduce the likelihood of a dog sustaining this painful injury and requiring surgery.
The first indication of inflammation, joint fluid thinning, is similar to a car's oil that does not perform optimally when it thins out. Joint fluid's primary role is to cushion the joint. It is thick and viscous and allows cartilage surfaces to glide next to each other smoothly as the joint flexes and extends under pressure.
When this cushion of joint fluid thins, the cartilage surfaces grind against each other. This results in the wear and tear of healthy cartilage and the release of chemicals that cause even more inflammation and further thinning of the joint fluid.
These chemicals that are released cause continuing breakdown of the CCL, allowing fibers to rupture bit by bit, until a partial or full CCL rupture has occurred.
Additionally, as cartilage wears away, an inferior cartilage matrix may develop to fill the gap, which is more prone to damage, and so the cycle continues.
Ideally, we want to find and stop this cycle of degeneration and inflammation as soon as possible. The test I show you in the video is the perfect way to identify the problem so we can break the cycle early.
They can be performed by veterinarians and pet parents, alike, so be sure to watch as I explain exactly what to look for.
If you aren’t a subscriber, be sure to sign up now HERE so you get the latest updates straight to your inbox, and always feel free to pass along to anyone who might benefit from this info!
Consider Cavaletti Jacks for Great At-Home Strengthening and practice
How to Prevent The #1 Cranial Cruciate Ligament (CCL) Complication
There is an often overlooked CCL injury and/or surgery complication. Because most people don’t know about it , it goes untreated and increases the chance that the dog will tear their other CCL 12-18 months after they tore the first.
We’ve been talking about issues related to and how to prevent cranial cruciate ligament (CCL) tears. Today, we’re continuing the CCL discussion, but I want to introduce the number one complication related to CCL surgery that is overlooked.
If I were to ask you to list the most common surgical complications, you’d likely come up with infection, hemorrhage, shock, blood clots. These are common and problematic. But when we talk about cranial cruciate injury or surgery, there is something we must specifically look for because unless we do something to stop it, every dog that has a cranial cruciate injury or surgery has this happen. And when it does, it increases the chances that the other cranial cruciate ligament will be injured.
The #1 cranial cruciate injury or surgery Complication is Range of Motion Loss
The most common things we see with CCL injury or surgery is loss of flexion of the hock and extension of the stifle. This may not seem like a big issue, but it can lead to something much worse. It can be a factor in the tearing of the opposite CCL. Remember, 25-50% of dogs that tear one cruciate will tear the other in the next 16 months.
It makes sense, every time a dog sits, they flex their hock. When they flex the hock, the tibia is pushed forward, straining the cranial cruciate ligament fibers. If some of the fibers are torn, it puts added stress on the remaining fibers, causing pain. If the whole ligament is torn, it puts abnormal stress on the joint capsule as the tibia slides forward, also causing pain.
To prevent the pain, dogs will decrease the amount they are willing to flex their hock. To keep the hock at 90 degrees instead of 30-45 degrees of flexion, they will hold the limb forward as seen by the tip of the toes being ahead of the other side. They will hold the leg out to the side, and they may externally rotate the leg with their toes pointing out. They then shift their weight off of the leg which had the cruciate injury onto the other side. The healthier leg is held medially, or toward midline when standing, has added weight on it when they are sitting and laying down, and has added stress at the joint when they rise into a stand. This puts added stress on the knee on the good side, causing inflammation. It is the inflammation that causes stress to the cruciate ligament that can then cause the sprain or tear on the good side.
Early warning signs of trouble in the “good” knee
Thinning synovial fluid and then effusion. In this series we will discuss how anyone can check for effusion and the most sensitive way to assess for thin joint fluid. Watch for that post.
How to Assess and Treat Range of Motion IssueS
Assessing a dog’s range of motion is easy with a Goniometer. With some specific manual therapy and/or some passive range of motion exercises, we can keep available motion in the normal range or return it to normal quickly when it is lost. I touch on this briefly in this video, but will go more in depth in a couple weeks.
How to perform passive range of motion correctly
It is super important to work on flexion and extension of each joint independently to prevent putting excessive strain on some of the joints without benefiting the restricted joints. Some joints may be hypermobile (having too much motion) and they can actually become even more hypermobile or overstretched, to compensate for the hypomobile joint (a joint that has restricted motion) when several joints are motioned at the same time. This can lead to an injury at the hypermobile joint and not change the range of motion of the restricted joint. We never want to stretch a joint in the direction of its hypermobility. We do want to perform passive range of motion if there is restricted motion, to normalize it.
We always want to work within the dog’s comfort level.
There are rare instances that we want to increase tarsal extension. If this is done indiscriminately, we can cause irreversible damage.
The 90 Second Rule
To increase flexibility (muscle related) or range of motion (joint related), we stick to the 90-second rule. That means flex or extend the joint that has lost flexion or extension in either two sets of 45 seconds, three sets of 30 seconds, or my favorite, 10 sets of 10 seconds. I know this adds up to 100, but it’s easy to remember and works really well.
If you aren’t a subscriber, be sure to sign up now HERE so you get the latest updates straight to your inbox, and always feel free to pass along to anyone who might benefit from this info!
Consider Cavaletti Jacks for Great At-Home Strengthening and practice
How to prevent Another Cranial Cruciate Ligament (CCL) Tear
Second CCL tears are unfortunately a huge problem for dogs that have already had one. In this Learn & Go, I show you how to spot issues and more importantly, what can be done to prevent second tears and surgeries.
Time to talk about Rio again. If you missed the last Learn & Go, Rio is a 10 year old Border Collie who was doing Agility and Flyball his whole life until he tore his right cranial cruciate ligament (CCL). He had surgery five months before I saw him, but hasn’t been the same since.
Rio had a typical post-cruciate “sit.” That is to say, the injured side was externally rotated, pushed forward, and there was a significant reduction in knee and hock flexion. All dogs, even Border Collies who have some external rotation in their hind limbs, should sit with their hind limbs well bent at the hock and stifle with the limbs tucked under them. Rio clearly held the affected limb abnormally.
We knew Rio was at risk of tearing his good CCL because he was overusing his good leg while he was off weighting his surgery leg. This is common after a CCL tear because the other limb ends up holding most of the weight when standing, walking, and rising from a sit or down position.
In Rio, there were already changes in his good knee that were warning signs. He had effusion, an indication of inflammation, which is the first sign of trouble. It can be reduced with supplements, possibly medications, and specific treatments, including ice, laser and Pulsed Electromagnetic Field (PEMF) therapy. But, the most important steps are to reduce the excess weight bearing on this limb and to strengthen the structures around this joint.
During his assessment, I found other complications, including back pain, elbow tenderness, and inability to stretch the biceps brachii muscle on both sides. His biceps can get excessively tight while he pulls his weight forward and over uses his front legs. As he continues to overuse his front end, we may see continued or additional areas of damage. If this happens, he will likely become less active overall as his compensations are now part of the problem. He can develop generalized atrophy and discomfort.
We were able to make him more comfortable immediately. I gave him exercises to do at home to strengthen the muscles that support the knees, hocks and elbows. We also worked on improving his range of motion at the tarsus so he can use his surgery leg appropriately, bending it underneath him, allowing for him to lift from a sit using that leg. All of these exercises will ultimately balance all 4 limbs bringing him back to a level of strength he had before the surgery.
Watch the video below all the way to the end. The last slide has great pictures of him after treatment, definitely worth watching for.
Consider Cavaletti Jacks for Great At-Home Strengthening and practice
Diagnosing and Treating A Dog’s Tarsal INjury
Rio, a 10-year-old Border Collie, came to me with some lameness. What was at the root of his issues? I’ll explain how I spotted it and how I treated him.
Let me introduce you to Rio, a 10-year-old Border Collie who went from being active and highly competitive in agility and flyball to slowing down considerable.
Rio’s dad drove 6 hours to see me; I had to find and fix his problems.What I found was not what we expected.
It's common to lose flexion of the hock on the same side as a cruciate rupture, but in Rio’s case, his other hock was a mess. Being that this was his good leg and most of his weight was shifted on to it, we needed to find a way to make it better.
I'm not going into his primary issue in this video (that will be the next Learn & Go). Today I'm showing you how easy it can be to miss something big, how to spot it and treat it.
In Rio’s case, effusion (abnormal collection of fluid) of the hock was visible, but this is not always the case. Take a look at the X-rays in the video to understand what you can look for.
Laser for Inflammation
Laser is always a great go-to when faced with inflammation. In Rio’s case, I was able to decrease the size of his hock by ~30%. There wasn’t complete success, however, because of bony or hard fibrous tissue changes.
Adding in Traction and A Mulligan Technique
Range of motion and discomfort were still an issue until we used traction and a Mulligan Technique. See 2:15 in the video to learn more about traction and 2:55 to understand the Mulligan Technique.
Strengthening After Treatment
Once pain is gone and the range of motion is back to normal, we need to strengthen the muscles, tendons and ligaments to prevent further injury.
Cavaletti Jacks are the perfect piece of equipment for strengthening the hock because you can set the height and distance for maximum hock flexion.
Incline sitting in another exercise that helps hock flexion and unilateral side strengthening. If you watch the video, you’ll see me demonstrate with my dog, Ollie, using our OctoBoard on four different levels so you can see how gravity affects his body.
Supplements for Musculoskeletal Support
Canine Musculoskeletal Support from Standard Process and good collagen will provide the support dogs need to heal even better and stay healthier for longer.
Order your own set of Cavaletti Jacks
Dr. Laurie Featured on the Petability Podcast
This week, Dr. Laurie was featured on the PetAbility Podcast with Cathy Symons CVT, CCRP, and Chris Cranston MPT, CCRP.
How to Improve your Geriatric Dog's Healthspan & Lifespan – with Dr. Laurie McCauley
This week, Dr. Laurie was featured on the PetAbility Podcast with Cathy Symons CVT, CCRP, and Chris Cranston MPT, CCRP, to talk about geriatric dogs and using an exercise program to extend their optimum life.
She answered the questions
When is my dog geriatric?
What happens to my dog's body and brain with aging?
How can I positively prevent or reverse some of the natural effects of aging?
How to perform Rhythmic Stabilization, one of Dr. McCauley's Top 5 Exercises for Geriatric Dogs.
Signs to look for before, during , and after exercise
How to create an exercise program for your dog?
What is Myos and how can this supplement help build muscle?
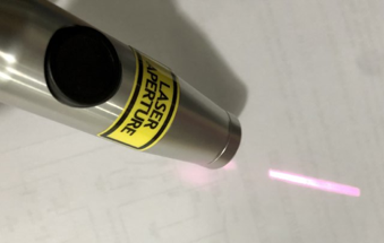
The most common laser mistakes – #1
In this series I’m covering The 5 Most Common Laser Therapy Mistakes. If you’re not getting amazing results with your laser you should listen
The number one mistake I see most often is…aiming.
It’s not too surprising given that most manufacturers instruct users to place the laser perpendicular to the skin, which is absolutely true if you’re not in contact with tissue. BUT, once you have contact with tissue, aiming makes all the difference.
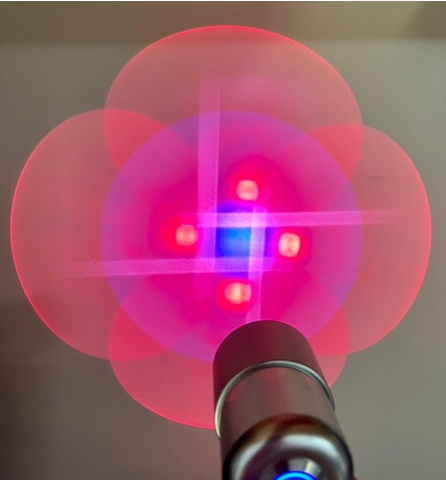
Did you know if you shine most lasers on a special surface (see below) you can see the beam that comes out of them?
Why aiming matters
Once the laser energy enters the tissue, there is refraction or scatter, meaning that the surface size of the treatment area expands, yet the tissue directly under the laser gets significantly more energy than the tissue around it. If you are treating a specific area, such as an OCD lesion or the cranial cruciate ligament, changing the probe’s position and the aim will significantly change how much energy gets to the target tissue.
Treating the cruciate ligaments
You can target the laser energy to have a direct effect on the cranial cruciate ligament. One way is to treat from the back of the stifle, through the popliteal fossa, aiming your beam and fanning the line of the CCL.
Treating the menisci
Feel the joint line and aim your light energy along this line to treat directly into the menisci on the cranial, caudal, and at least medial surfaces. Most meniscal tears are in the medial meniscus. If there is a lateral tear, or if you are not sure if there is a tear, treat the lateral surface as well. By aiming directly on the joint line, parallel to the meniscus line, significantly more energy will be absorbed by the menisci than if there is an angle to the probe and the energy has to pass through bone.
Are you feeling like there is more to using a laser machine than turning it on and pointing at the tissue you want to treat?
There absolutely is!! We want to help you have optimal outcomes with all of your patients, and that comes with a better understanding of what is going on in the tissue and how the laser can affect it. Improving your outcomes leads to happier clients and believe it or not, improved job satisfaction. We have had hundreds of veterinarians take the Optimum Laser Therapy course and rave about how much it has helped them and their patients.
The most common laser mistakes – #2
In this series I’m covering The 5 Most Common Laser Therapy Mistakes. If you’re not getting amazing results with your laser you should listen
Have you ever watched someone pick up a laser they weren’t used to using expecting the same results from their normal go to? Maybe that’s been you.
Different lasers have widely different treatment (dosing) parameters depending on the variables of the laser. Using the wrong dosing unintentionally means your patient isn’t being treated properly. They could get no effect from the treatment, they could fell discomfort or in worst case scenarios, the laser can hurt the patient.
Let’s get into the variables.
The SECOND mistake I see most often is not knowing the variables of the laser.
Hopefully after watching the video your interest is piqued, and you will investigate your laser.
The power of LEDs
LEDs in the 600nm range can be used to heal corneal ulcers, wounds and burns; they can a be great for treating acupuncture points, anxiety and depression, and strokes. They may not, however, perform as well in treating arthritis, according to current research.
High Wavelengths
980 nm wavelength lasers have been shown to have significant effects when treating dogs with degenerative myelopathy and elbow arthritis. In fact, research has shown that when using this wavelength,10-19 J/cm2 had optimum effects when treating elbow arthritis. If you were to use that dosage with some of the other wavelengths there would be deleterious effects.
Considering your patient’s skin color
Melanin has to be considered when treating in the 800nm wavelength range because it absorbs a significant amount of laser photons in the range, and the tissue will heat up more than we want if the appropriate amount of energy is delivered too quickly.
Power with Pulsing
When looking at power of the laser machine, any laser that has 904nm or 905nm will need significant Peak Power. You may see 36 W, 50W, 75W or even 100W of peak power.
That is because in order to deliver this wavelength without severely heating the tissue it, needs to be either chopped (i.e., on 50% of the time, then off 50% of the time), or super-pulsed (i.e., on for nanoseconds, then off for a proportionally longer time). We usually need the least amount of total energy to have a significant effect with this wavelength.
Are you feeling like there is more to using a laser machine than turning it on and pointing at the tissue you want to treat?
There absolutely is!! We want to help you have optimal outcomes with all of your patients, and that comes with a better understanding of what is going on in the tissue and how the laser can affect it. Improving your outcomes leads to happier clients and believe it or not, improved job satisfaction. We have had hundreds of veterinarians take the Optimum Laser Therapy course and rave about how much it has helped them and their patients.
The most common laser mistakes – #3
In this series I’m covering The 5 Most Common Laser Therapy Mistakes. If you’re not getting amazing results with your laser you should listen
It’s been said that expectations are the precursor to disappointment. Maybe that’s true with some things, but laser therapy is not one of them.
With laser therapy, expectations are extremely important. And not having them is the third top mistake I see professionals make. What are the other expectations we should be looking at; they are equally important? In this video, I walk through what to expect when targeting muscles, nerves, tendons, wounds and burns, discolored tissue, and urethras.
Not knowing what to expect is the 3rd top mistake that I see
Without an understanding of what to expect with a laser, you are likely not getting what you could. It’s similar to getting into a Ferrari with the belief that it drives just like any other car. Sure you can drive it that way, but you will be missing out on a lot of performance.
A clear understanding of what you’re treating and what you’re measuring is key with laser Therapy
If, for example, you are only looking at pain management as the parameter with your treatment, then you may not be watching at how quickly the wound you are treating is healing. You could also miss noticing that the effusion in the stifle is gone (remember it is chronic inflammation in the stifle that is the biggest predeterminer of a torn CCL).
High Doses vs. Low Doses of energy
With laser therapy, high doses of energy are used to treat pain because it decreases ATP production, which reduces nerve impulses and creates a form of an axonal nerve block. But that high dose of laser energy does not actually aid healing. It has been shown that high doses of laser energy have been shown to reduce fibroblast migration.
Lower doses of energy, on the other hand, may not have as big of an effect on pain, but it can accentuate healing because it helps to increase ATP in the targeted cells, which allows them to do what they need to do faster and more efficiently.
Knowing your goal to set your dosing
In short,
Pain calls for higher doses
Tissue healing calls for lower doses
Learn more about laser power and ATP production in this Learn & Go.
The most common laser mistakes – #4
In this series I’m covering The 5 Most Common Laser Therapy Mistakes. If you’re not getting amazing results with your laser you should listen
Every year more research comes out on when to use laser therapy, which parameters have superior effects. Changes in power, wavelength, frequency, and total dosage can make significant changes in outcomes.
In one study, athletes were treated with laser therapy in four different situations: before working out with placebo after, before and after working out, after working out with placebo before, and placebo both before and after working out. Researchers found that athletes increased their endurance when they were treated both before and after working out. Strength, on the other hand, was built the fastest when athletes were treated before exercise and had the placebo after.
With so much that can be done with lasers, let’s make sure you’re doing everything right. Ready for the fourth most common mistake I see in laser treatment?
The #4 the most common laser mistakes covers dosing.
Using the wrong dosE is the 4th top mistake that I see
Laser manufacturers provide a dosing guidelines for each of their lasers, and this is always where you should start. They get a lot of input on the best dose for different ailments, but you will know what is going on with your patient on the day of treatment better than anyone else, especially the laser manufacturer.
Laser Tip
The easiest way to know when you need to add more laser therapy treatments or when to stop treatment earlier than recommended, is when dealing with trigger points. If the trigger point dissipates when you are treating, then ceasing treatment is a good option.
Get used to feeling the tissue before and after a treatment so you can quickly differentiate a trigger point that needs more energy from one that is resolved.
The most common laser mistakes – #5
In this series I’m covering The 5 Most Common Laser Therapy Mistakes. If you’re not getting amazing results with your laser you should listen
I have spent over 20 years studying, researching and working towards perfecting laser therapy, and I want to share some very important points with you that will help you improve your laser outcomes today.
Today we’re starting with #5 of the most common laser mistakes.
One of the most common laser mistakes I see Vets make is Not using their laser!
You would be amazed at how many vets say, “yeah, I've got a laser and it's sitting over there in the corner.”
But let’s get into why this isn’t working for them.
Everybody knows about the contraindications – the reasons not to use a laser. But some vets don't realize what all the indications are. So let's talk about both.
Contraindications
Cancer
Cancer seems like a clear contraindication. Except laser therapy can be a great treatment for palliative reasons.
Injection Sites
When we inject something into the tissue, it can have a direct effect or it can be metabolized, and the metabolites can have an effect in the body. The effects of the injection have been studied, so we have an expected outcome, but if laser energy, with or without heat, may change that outcome.
The substance may be altered and/or the tissue around the substance may be altered. We know there are effects on circulation, usually vasodilation and changes in the permeability of the blood vessels. The cells in the treatment field can have changes in electrolyte transmission through the cell membrane, and we may even affect cell messenger complexes. We just don't know how laser therapy can affect the injected substance or how it is metabolized, so for now, it is best to consider this a contraindication until we know more.
Indications - These are just a sampling of those you may not have thought of
Dental issues
Surgery healing
Osteoarthritis
Stroke
Nerve Regeneration
Kidney Perfusion
Bronchitis
Chronic Cystitis
Degenerative myelopathy
Behavioral issues
Cellulitis
Perianal fistulas
Snake bits
Anal glands
and more!
How the shape of a laser’s lens changes the beam and affects the power
Did your laser come with flat lenses, convex lenses, or both? Did you know that depending on the surface of the laser lens, and the distance the lens is from the tissue you are treating, there can be a huge difference in the amount of energy you are putting into the tissue?
Did your laser come with flat lenses, convex lenses, or both? Did you know that depending on the surface of the laser lens, and the distance the lens is from the tissue you are treating, there can be a huge difference in the amount of energy you are putting into the tissue?
Flat vs. Convex Lenses and the impact on power
Light energy flows through a convex lens in a converging manner, meaning it becomes more and more intense as it reaches its focal point. This focal point is where all of the energy that comes out through the lens is concentrated into a pinpoint size space if there is just one diode and into the most focused pattern if there are multiple diodes.
Different lenses treat tissues differently. A convex lens will provide the most energy in one place, making it great for precise applications, like when treating an acupuncture point. While a flat lens with a more diffuse and weaker beam is better when treating skin where the goal is to have minimal penetration.
Why do we need to know this information?
The more we know, the better effects we can have each and every time we use our lasers. and better effects mean better patient care, better outcomes, and better job satisfaction.
Learn everything you need to know about lasers in our Optimum Laser Therapy Course
〰️
Learn everything you need to know about lasers in our Optimum Laser Therapy Course 〰️
The Top Starter Exercise for Athletes
Learn the best exercise to start with athletic dogs. Understand how to perform it correctly, decrease the chance of injury, and help make Your dog, and your patients, stronger, faster, and smarter.
Do you have a canine athlete? Or do you work with canine athletes? If you answered yes to either of these questions, you are going to want to watch this video.
This is one of the first exercises I teach to all of my clients who have athletic dogs. And I guarantee you would be amazed at how many athletes can't do this exercise or can't do it correctly.
With the help of a peanut ball this single exercise strengthens the rear limbs, the core, and the front limbs. It also stimulates the brain in a way that very few exercises can.
In this video, I'll teach you how to choose the correct size ball, I explain the importance of the dog’s and your positioning, and I give viewers a sneak peek of what this exercise could lead to – the ninja dog.
Learn to perform this exercise correctly, decrease the chance of injury, and help make your dog, and patients, stronger, faster, and smarter.
If you have ever done ball work with a dog, you will find that dogs learn how to cheat. If you've never done ball work, then you likely don't know what to look for, giving your dog more room to "cheat" and maybe even setting them up to fail.
When done correctly, this exercise can strengthen a dog's whole body and engage the brain.
By strengthening the rear limbs in this manner, we are targeting the muscles for propulsion, power, jumping, and speed.
When done correctly, this exercise strengthens the muscles that support the carpal joints/wrists, elbows, and shoulders while putting less stress on the joints than if the dog were walking on the ground.
So many working dogs, especially agility dogs, have acute or chronic repetitive stress injuries of the carpal, elbow, and shoulder joints. This exercise allows us to strengthen the tendons and ligaments that support these joints without any of the stress seen with so many other exercises.
New Laser Study - Power, ATP & Oxidative Stress
Turns out that you need higher power when using a laser with a 980 nm wavelength to increase ATP production and decrease oxidative stress.
A recent study on different power levels and their effect on ATP production and oxidative stress had some surprising results.
We always want to increase ATP to help cells heal, or do whatever they need to do, better. Concurrently, we want to diminish oxidative stress, i.e., reactive oxygen species (ROS) or free radicals. The problem lies in the fact that when mitochondria make ATP, ROS are a byproduct.
In this study ATP production and ROS are measured when cells are treated with a laser with 980 nm wavelength with power levels of 0.1W to 1.1W in 0.1 increments. Watch the video below to see the results, you may be surprised!
MORE ON LASER
We have known for a long time the effects of therapeutic laser (photobiomodultion) on tissues. Laser treatment can reduce inflammation, improve blood flow, and reduce pain. We know that wavelengths from 400-1064nm can affect tissues. We know the overall mechanisms of how lasers work but in some cases we are still figuring out the specific details for each wavelength.
Mitochondria
As we know, mitochondria generate ATP, which is then used by the cell as a source of energy. Oxidative stress from ROS, which are generated during the metabolism of the mitochondria, is a by-product that cannot be avoided.
These ROS will uncouple the mitochondria, increasing the oxygen consumption. Overall, this makes the mitochondria work harder but not increase ATP production. A normal cell will have a balance of ROS and ATP production that will keep the ROS from further damaging the cell. However, a cell that has been affected by local trauma will become out of balance, the ROS production will go up and there will not be enough ATP to prevent further damage to the cell. By increasing the ATP production in a cell, balance, homeostasis, is returned to the cell.
The 980 nm wavelength is commonly used in several of the lasers we use in veterinary medicine. We know these lasers work, and as we can see from this study, we know we will need higher levels of power at our target tissue to have beneficial effects. With laser therapy we can definitely create those beneficial effects. By increasing the energy metabolism of the mitochondria, and therefore the ATP level, the oxidative stress is reduced and an unhealthy, out-of-balance cell can be moved back to health and homeostasis.
For the full article, see: Photobiomodulation and Oxidative Stress: 980nm Diode Laser Light Regulates Mitochondrial Activity and Reactive Oxygen Species Production